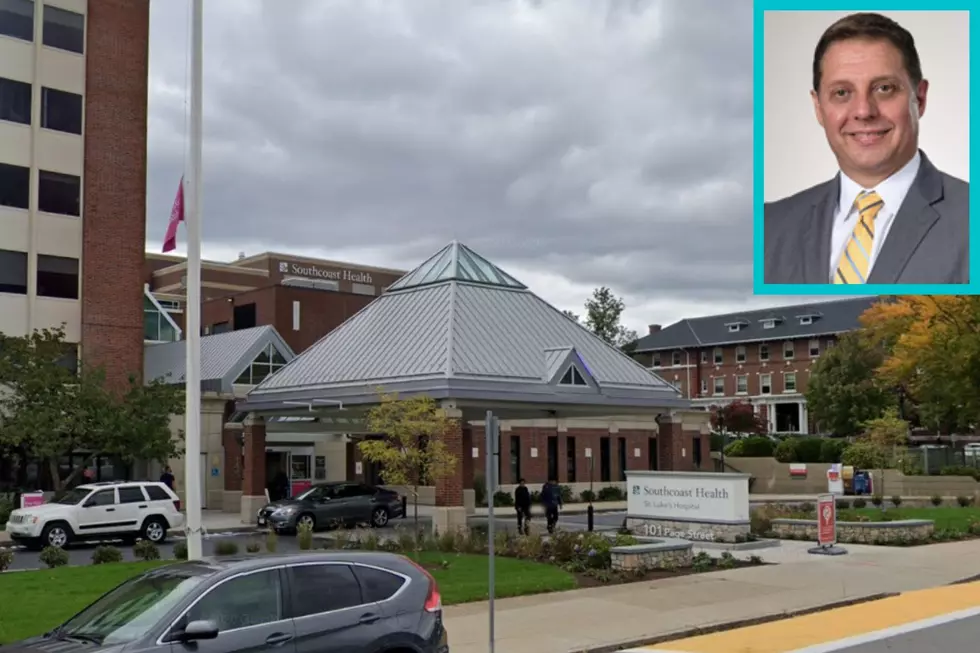
Southcoast Doctor: Respiratory Infections ‘Rapidly Rising’
NEW BEDFORD — As the holidays roll on and winter enters its second week, respiratory illnesses are increasing across the country — and the SouthCoast is no exception.
That's according to pulmonary critical care doctor and Chief Clinical Officer for Southcoast Health hospitals Dr. Dani Hackner.
Dr. Hackner said earlier this month that healthcare professionals are "concerned" with the numbers — and that excess mortality is seen during COVID peaks, along with increased risk of heart attack and stroke for those who recover from the virus.

Tripledemic on the SouthCoast
Dr. Hackner said before the holidays that there were dozens of COVID-19 patients at St. Luke's Hospital, with fewer than half coming in for the virus but testing positive during their stay.
"Those numbers have been stable for the past month," he noted, adding that there have been increasing community cases as well as a rise in other respiratory infections.
This season, COVID transmissions have hit at the same time as flu and respiratory syncytial virus, known as RSV, in what many are calling a "tripledemic."
According to Dr. Hackner, the SouthCoast is seeing unusually high numbers of flu cases and cases of RSV beginning as early as the summer.
“We’re also seeing non-flu, non-COVID, non-RSV respiratory cases increasing," he added. “The short story is, a lot of these bugs have missed us during COVID.”
With immunity to other illnesses lower after two years of widespread masking and social distancing, the population is now more at risk of catching respiratory viruses.
Getting vaccinated against COVID and flu is "a major factor in reducing mortality," Dr. Hackner said.
Long COVID and Risk of Heart Attack or Stroke
Dr. Hackner said Southcoast Health hospitals have seen stable mortality rates over the past six months.
"But there is no doubt during the peaks of Covid, we saw excess mortality," he said, adding that the high number of deaths were likely in part due to comorbidities and undervaccination.
New studies show that a COVID infection — even mild ones — can also increase the risk of heart attack and stroke.
According to Dr. Hackner, the research corroborates what healthcare workers have seen during COVID peaks on the SouthCoast.
“We also saw peaks of acute myocardial infarction and stroke during those times," he said. "Though they were small peaks, it does support what’s been observed in the literature."
The increased risk of cardiovascular events in COVID patients could be due in part to patients having underlying comorbidities that are exacerbated by the virus, or having secondary issues after a COVID infection, Dr. Hackner noted.
Although it is not yet well understood, "long COVID" seems to describe patients who recovered from acute illness but continue to experience persistent symptoms afterwards.
"Those symptoms most commonly are generalized, in terms of fatigue, deconditioning, shortness of breath," Dr. Hackner said.
"But they can also include cough, and chest tightness, neurologic symptoms, psychologic symptoms, functional difficulties that are quite pronounced, and so forth."
Southcoast Health doesn't run a centralized COVID clinic where data from patients with long COVID symptoms is tracked — rather, each patient is seen according to their particular symptoms, Dr. Hackner said.
"Frankly, the literature is still unclear whether long COVID is a single entity, or is a set of entities in the wake of severe, critical illness," he noted.
"But it’s entirely possible that bumps in either stroke or cardiac injury or even pulmonary embolism during peaks of COVID may be directly related to the disease," he added. "We just don’t know."
Main Concerns
In general, Dr. Hackner said COVID outcomes on the SouthCoast over the past six months have been "very good in terms of mortality and complications."
But healthcare professionals are still concerned that patients put off necessary testing or treatments during the pandemic.
"Our biggest concern is that patients stayed away from healthcare services during peaks of COVID," Dr. Hackner noted.
He added that accessibility of care and getting vaccinated against COVID and flu are extremely important.
"The biggest concern is access to care, especially in diverse populations," Dr. Hackner said. "We want to encourage patients, especially in this very difficult season with multiple respiratory conditions, to not delay access in care."
Top SouthCoast Stories on WBSM Dec. 19-25
Top SouthCoast Stories on WBSM Dec. 12 - 18
More From WFHN-FM/FUN 107




![New Bedford Community Health Center CEO Gives COVID Update [TOWNSQUARE SUNDAY]](http://townsquare.media/site/518/files/2020/03/outbreak-coronavirus-world-1024x506px.jpg?w=980&q=75)

![How New Bedford Should Handle the Rise in COVID Cases [TOWNSQUARE SUNDAY]](http://townsquare.media/site/518/files/2020/06/GettyImages-1215276619.jpg?w=980&q=75)

